COVID-19 deaths in aged care homes “not inevitable”, study of international measures to manage outbreaks shows – data and regular testing required
A useful record of what has been done so far by countries to tackle coronavirus in aged care. While aged care residents may be at higher risk from dying from coronavirus because of their co-morbidities and the difficulties in physical distancing in...
A useful record of what has been done so far by countries to tackle coronavirus in aged care.
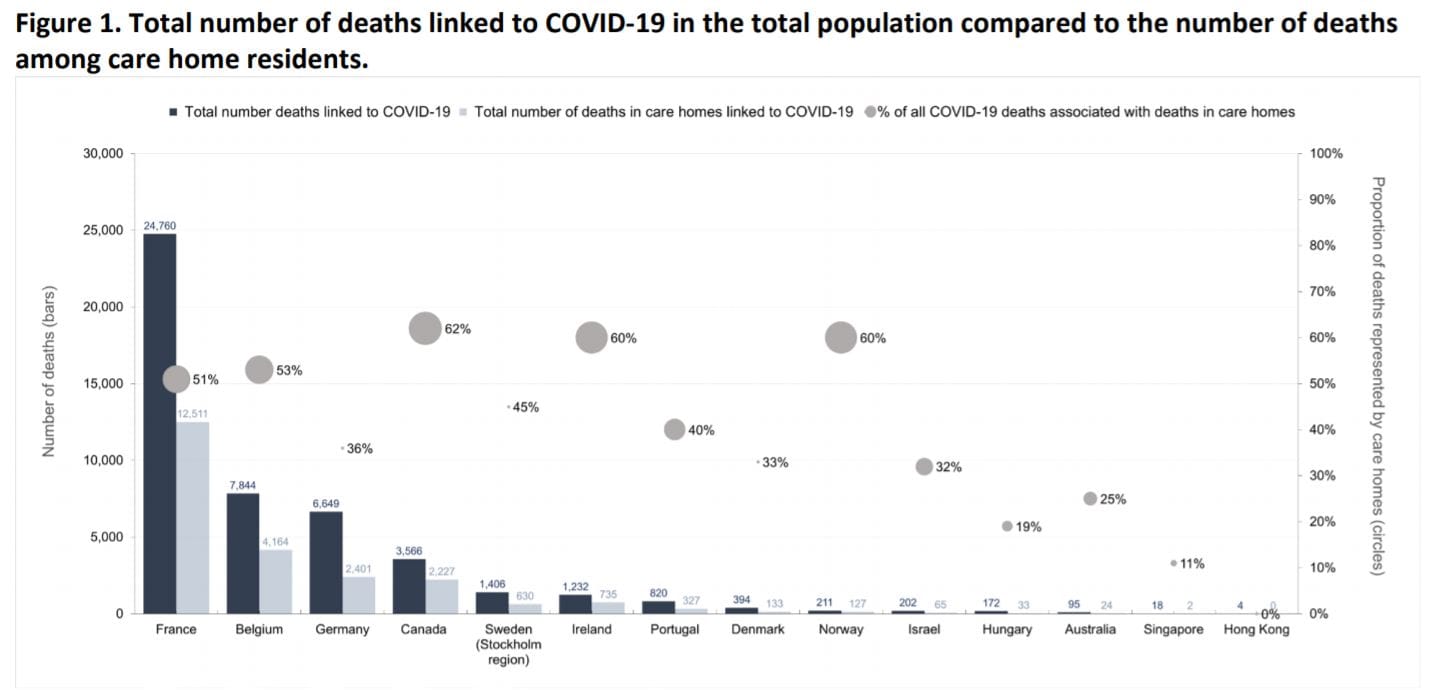
While aged care residents may be at higher risk from dying from coronavirus because of their co-morbidities and the difficulties in physical distancing in communal living, deaths can be avoidable, according to a recently published paper by the London School of Economics and Political Science.
The paper – by Adelina Comas-Herrera, Elizabeth C. Ashcroft and Klara Lorenz-Dant from its Care Policy and Evaluation Centre – looks at international examples of measures to prevent and manage COVID-19 infections in care – including in Australia and makes a number of key findings:
- A National Taskforce – including representatives from government departments and industry peaks – can ensure that the COVID-19 response in aged care homes is well coordinated with the other policies and measures in the community and health system.
- Countries need IT systems i.e. data that can be used to monitor outbreaks in and near aged care homes and are linked to the systems for pandemic planning and resource targeting. The researchers note that many countries left out care homes from national priorities for testing, allocation of Personal Protection Equipment (PPE) and even out of the counts of COVID-19 cases and deaths (including the UK and Italy).
- The asymptomatic nature of COVID-19 renders most training and guidance in infection control “not suitable” – documents must be reviewed and updates to include the latest evidence on the virus.
- Rapid response teams are required to tackle outbreaks in aged care homes because of the risk that homes will be left short-staffed if a high number of staff become ill or need to self-isolate.
- Care homes need to be supported in assessing the effectiveness of isolating residents in their current buildings. “If more isolation spaces are required than can be provided, contingency plans should be put in place, such as using adapted hotels or other accommodation,” the researchers say.
- Restricting visits to aged care homes by families, except in end-of-life situations is not always enough to prevent infections coming in from outside so visiting must be made safer through the use of PPE and physical distancing. Staff should also ideally only work in one home, and one area of the home, with sick pay ad alternative accommodation offered. In addition, all new residents should be isolated and tested.
- Residents and staff should be regularly tested (particularly where there are local cases of COVID-19 in the community), with contact tracing of staff and residents and isolation implemented when positive cases are detected. “Once a case of infection has been detected, all other residents and staff who have been in close contact with them should be considered as possible cases of COVID-19 and should isolate until test results can confirm whether or not they have the infection. Symptom monitoring (and ideally testing) should be done for all other residents and care staff.”
- Care homes should be divided into risk zones for possible, probable and confirmed cases, and staff should only work in one of the zones. “Where the facility layout and space does not make this possible, isolation outside the facility should be considered,” they state.
- Access to healthcare and palliative care (in terms of personnel, medicines and equipment) needs to be guaranteed, particularly for homes without nursing or medical staff.
- Measures to address the psychological impact of the pandemic on both staff and residents need to be put in place, as many will have experienced trauma and grief. “For some residents, particularly those with dementia, the disruption in their normal lives by the measures may have significant negative impacts,” the researchers conclude.