Opinion: Residential Aged Care Costing Study fails to capture real cost of care
A new study for the Independent Health and Aged Care Pricing Authority (IHACPA) has underlined the need for a fresh approach to residential aged care funding – one that takes into account Plan B or increased consumer contributions.
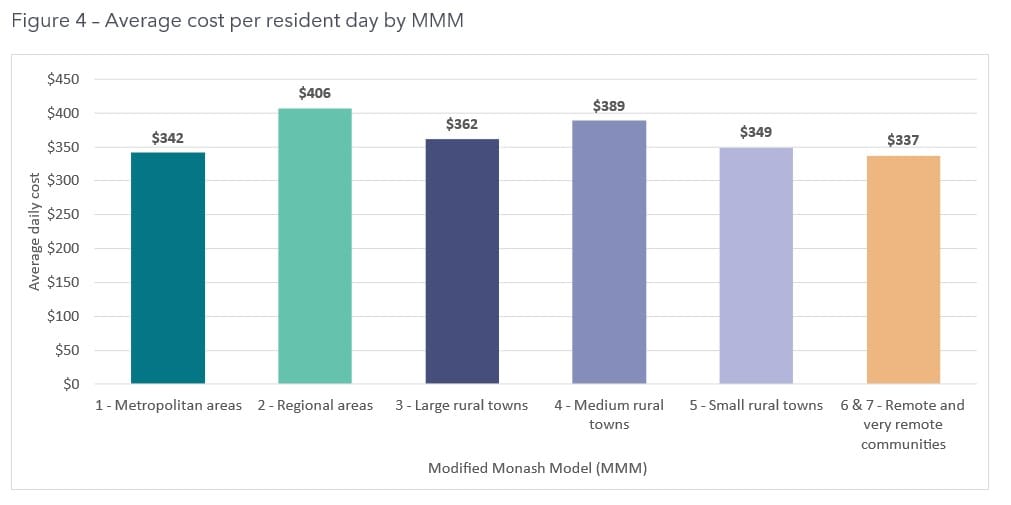
A new study for the Independent Health and Aged Care Pricing Authority (IHACPA) has underlined the need for a fresh approach to residential aged care funding – one that takes into account Plan B or increased consumer contributions. As we reported last week, the newly released 2023 Residential Aged Care Costing Study by Scyne Advisory (formerly PricewaterhouseCoopers) commissioned by IHACPA found the average cost of residential aged care per resident per day was $352. However, a closer look at the numbers contained in its report reveals that this figure includes the Basic Daily Fee, additional services and accommodation and hotelling supplements. So, providers needed to be pulling in $352 per resident per day of taxpayer and consumer funding across the board just to break even. Doing a quick comparison with the StewartBrown Aged Care Financial Performance Surveys for the same period as the study, the cost of care is virtually the same – but there are a few key differences.
Data now out of date
One of course is the sample size – 111 facilities or around 4% of the industry compared to the 1,200-plus homes typically surveyed by StewartBrown. Unlike the StewartBrown surveys – which Scyne drew on for part of their financial data – the study also includes Government-run homes, which tend to operate under a more clinical care model and therefore run at a higher cost – $443 or $95 more than the $348 recorded by For Profit and Not For Profit facilities in the study. The financial data was also collected in the second and third quarters of 2022-23 – so before the Fair Work Commission (FWC)’s 15% wage rise for direct care workers and the 5.75% minimum wage rise, and the 1 October 2023 requirements for 200 mandated minutes of direct care – all of which have increased labour costs for providers significantly. In short, the study is now out of date – and doesn’t necessarily reflect what the true costs of residential aged care are for most operators today.
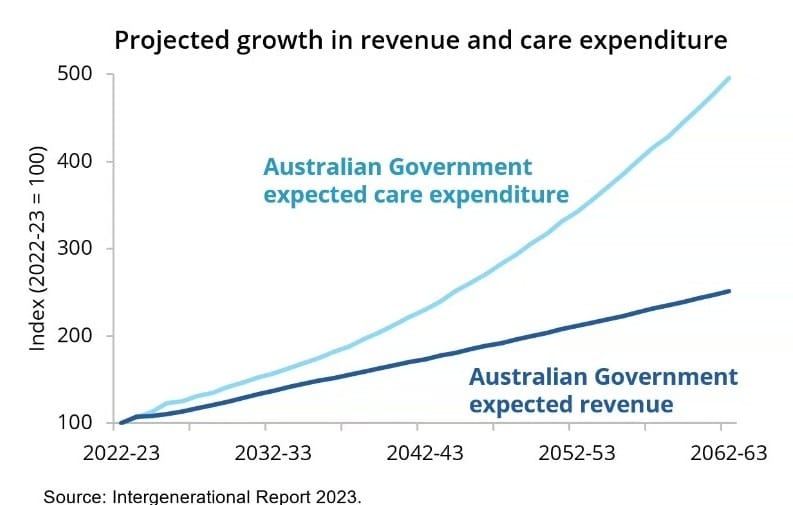
Plan B needs to be part of the pricing discussion
Worryingly, the report states that the study will be used to inform the 2024-25 AN-ACC price – due to be announced in August and start from 1 October this year. You have to ask the question: should IHACPA’s focus instead be on what is high-quality care – and what will be required to deliver this under the future Aged Care Act – rather than what was being provided last year? If we talk about the cost of care in terms of what will be required in the coming years, then increased consumer contributions from those with the means to pay – or Plan B – has to come into the equation. Looking at the StewartBrown data from the same period as the Scyne study, they noted that residential care operators were losing over $16 per resident per day at the time. This gap in profitability can only be bridged by consumers with the means to pay – with a suitable safety net in place for those who cannot. Will the Aged Care Taskforce’s Final Report – due out any day – give Plan B the tick of approval – and will IHACPA take this into consideration as they weigh up this year’s price?