Professor Joseph Ibrahim says aged care sector’s performance during COVID-19 has not “washed away” Royal Commission – improvements needed now before second and third waves
You can read the full 1,400-word piece here
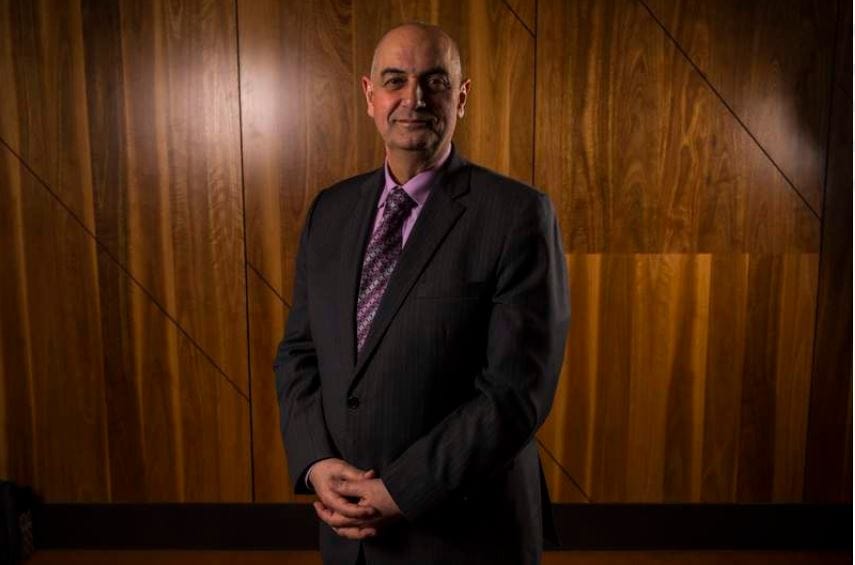
The always-outspoken Monash University Professor has delivered yet another warning – this time that there are still severe issues in the sector that need to be urgently resolved before the fatality rate among aged care residents goes up – in an editorial for the Australian Journal of Advanced Nursing (AJAN) July-August issue. You can read the full 1,400-word piece here. He says the strong result of the sector is because of geography, not because of good work by the sector. “The absence of catastrophic impacts of the COVID-19 pandemic in aged care homes in Australia that occurred around the world are not evident of a highly functioning system,” he writes. “The virus has not washed away the systemic failures highlighted in the interim report by the Royal Commission into Aged Care Quality and Safety.” Professor Ibrahim says there are five issues that need to be addressed if Australia is to avoid the high COVID-19 fatality rate among aged care residents seen in other countries:
Governance:
He argues the 1. Government was too slow to recognise the risk of COVID-19 to older people or
- the multiple authorities involved including the Aged Care Quality and Safety Commission and the Department of Health.
“This hampered development of a coherent policy and appropriate practice for a humane lockdown at each aged care facility.” “At a local level there was confusion for aged care providers and staff when an outbreak of COVID-19 occurred such as at Newmarch House.” He adds that better transparency – and public reporting – about the care of residents would have eased this situation.
Workforce:
Professor Ibrahim says the Government was slow to recognise that the sector was understaffed and not equipped to provide the same level of acute care as hospitals despite its funding for a ‘surge’ workforce. He adds that the expectation that personal care workers should ‘step up’ is unreasonable and unfair – “This issue should have received a more robust public, aged and health care sector debate.”
Models of care:
The Professor notes that the emergency response to the pandemic assumed aged care providers could offer acute care and says the future system must resolve the issue of aged care as a home or a hospital. “The older person in an aged care home has a diverse set of clinical, health maintenance and quality of life needs. The expertise for all aspects is unusual to find in one place.”
Evaluation, including the use of data:
Professor Ibrahim says while the amount of data around COVID-19 has been overwhelming, there has been little useful information to guide aged care – mostly because this data was not being collected or if gathered, not released, prior to the pandemic.
Resources and infrastructure:
The Professor highlights that the design of many existing aged care homes contributed to difficulties in maintaining infection control – small bedrooms, shared bathrooms, and communal areas etc. Like the Royal Commission, he concludes that the sector needs “transformation” now – but may lose out to the Government’s other priorities without strong advocacy for change.